Department Introduction
Neurosurgery | Excellence
:::
Excellence
Awards
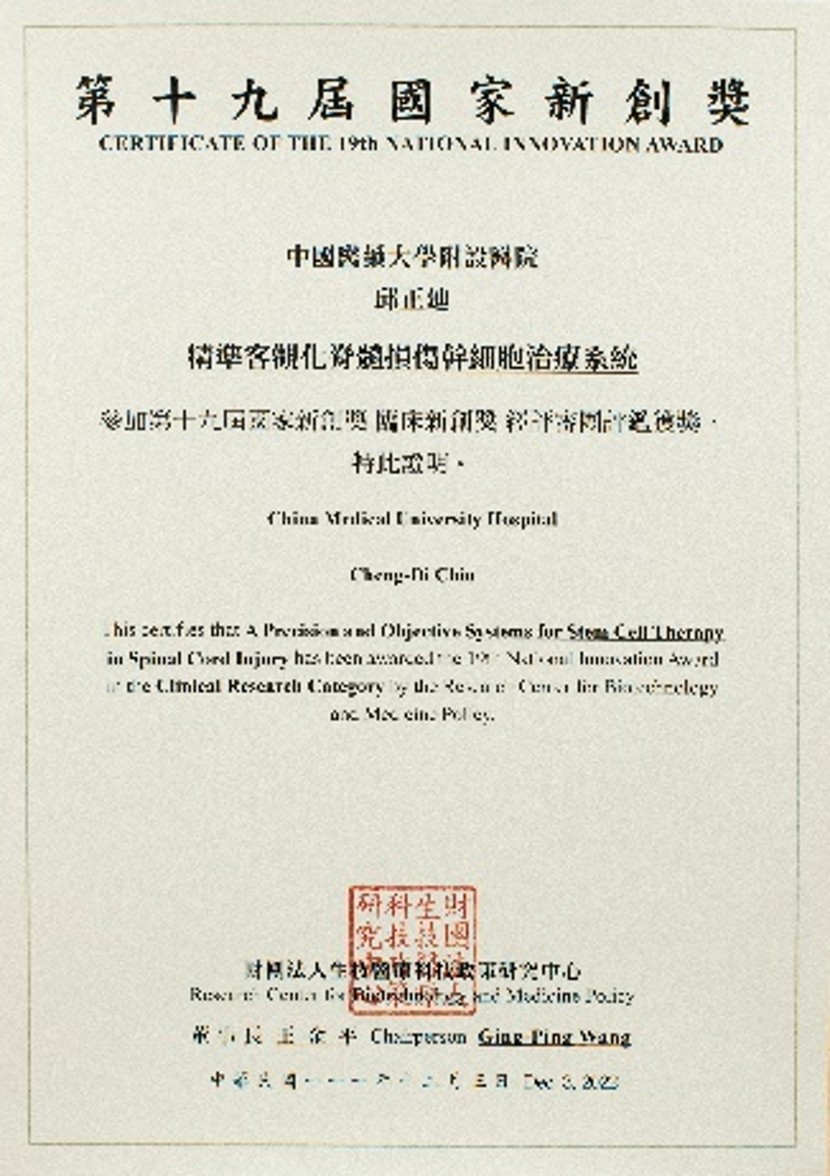
Dr. Cheng-Di Chiu: National Innovation Award for the precision spinal cord injury stem cell treatment system (2022)
This system combines autologous bone marrow mesenchymal stem cells, navigation systems, and image processing technology for accurate stem cell placement and medical imaging assessment, improving the precision and objective evaluation of spinal cord injury stem cell treatments.
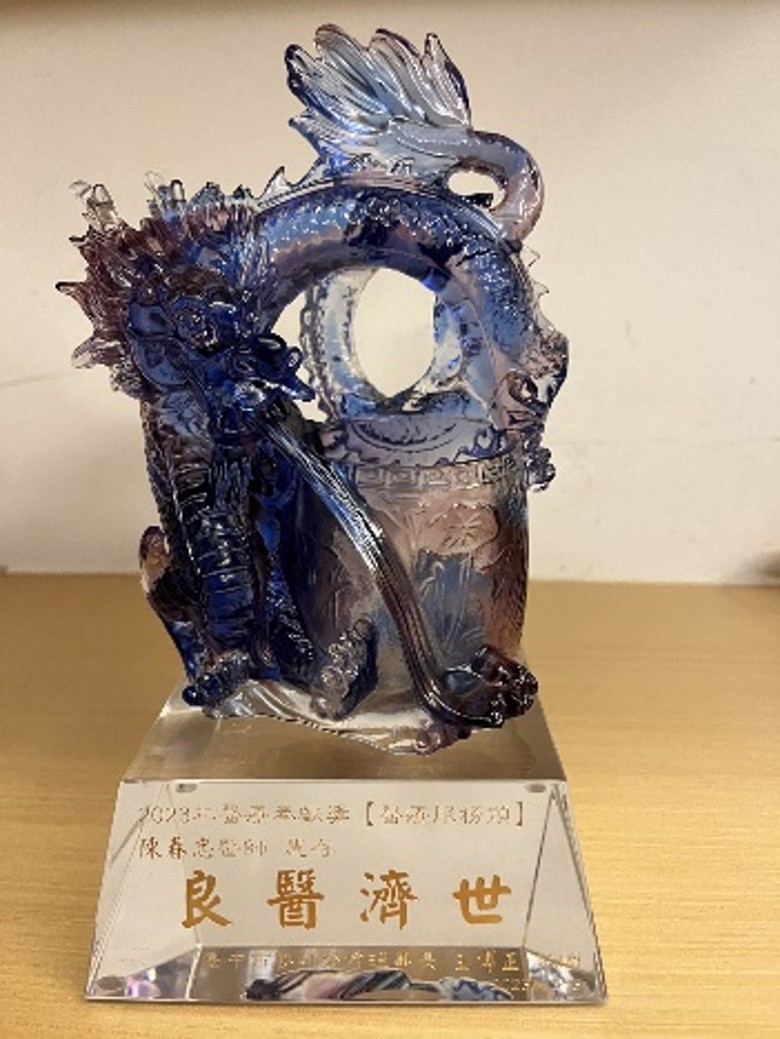
Dr. Chun-Chung Chen: Taichung City Medical Association - Medical Service Award (2023)
Dr. Chun-Chung Chen specializes in the challenging fields of cerebrovascular diseases and brain tumors. He not only seeks to advance surgical techniques but also engages in clinical research to provide patients with the latest and most effective care.
▲
